More Information
Submitted: December 29, 2025 | Accepted: January 06, 2026 | Published: January 07, 2026
Citation: Hasan R. Chilblain Lupus Erythematosus in an Adult Female: A Case Report. Ann Dermatol Res. 2026; 10(1): 001-003. Available from:
https://dx.doi.org/10.29328/journal.adr.1001038.
DOI: 10.29328/journal.adr.1001038
Copyright license: © 2026 Hasan R. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Chilblain lupus erythematosus; Cutaneous lupus erythematosus; Acral lesions; Cold-induced rash; Perniosis
Abbreviations: CHLE: Chilblain Lupus Erythematosus; SLE: Systemic Lupus Erythematous; CLE: Cutaneous Lupus Erythematous; ANA: Antinuclear Antibodies
Chilblain Lupus Erythematosus in an Adult Female: A Case Report
Reem Hasan*
Department of Dermatology, Damascus University, Damascus, Syria
*Corresponding author: Dr. Reem Hasan, MD, Department of Dermatology, Damascus University, Damascus, Syria, Email: [email protected]
Background: Chilblain Lupus Erythematosus (CHLE) is a rare, chronic subtype of Cutaneous Lupus Erythematosus (CLE), typically affecting acral sites during cold weather. Its clinical and histopathological overlap with other conditions often leads to misdiagnosis.
Case presentation: We report a case of a 35-year-old Middle Eastern female from Syria, who presented with recurrent erythematous lesions on the face and acral areas exacerbated during winter. Initial diagnosis suggested Discoid Lupus Erythematous (DLE) based on skin biopsy. Further clinical evaluation and laboratory investigation confirmed CHLE. The patient responded remarkably to topical corticosteroids and cold protection measures.
Conclusion: This condition should be considered in patients with recurrent acral lesions triggered by cold exposure. This case underscores the importance of distinguishing CHLE from perniosis and other CLE subtypes through thorough clinical and histopathological assessment.
Chilblain Lupus Erythematosus (CHLE) is a rare, chronic subtype of Cutaneous Lupus Erythematosus (CLE), typically manifests on acral sites during cold weather [1]. CHLE lesions closely resemble those of perniosis, which represents the main differential diagnosis [1]. However, due to its rarity, it may be misdiagnosed as perniosis, especially since the lesions are predominately located on acral sites and tend to worsen in winter. Misdiagnosing with other forms of Cutaneous Lupus Erythematosus in particular Discoid Lupus Erythematosus (DLE) is also possible because of the overlapping cutaneous manifestations and histopathological features. Hence, we highlight the importance of detailed examination as well as histopathological and laboratory investigations in suspicious cases to make the accurate diagnosis. Here, we present a case of CHLE in an adult female who fulfilled both the major and minor diagnostic criteria for this disorder.
A 35-year-old middle eastern woman from Syria, presented with a recurrent skin rash located on the face, hands, and feet. The patient reported that this rash appeared spontaneously in winter and regressed during summer and hot weather and these lesions were pruritic and painful. She reported no systemic symptoms, had no significant medical or family history, except for she had previously been misdiagnosed with DLE and was treated accordingly with hydroxychloroquine 200 mg daily.
On physical examination, the patient had an asymptomatic malar rash on the face, which was subtle due to her darker skin tone, along with multiple erythematous papular lesions on the hands and chilblain-like lesions on the feet (Figure 1).
Figure 1: A- Malar rash on the face. B- Multiple popular lesions on the hands. C- chilblain-like lesions on the feet.
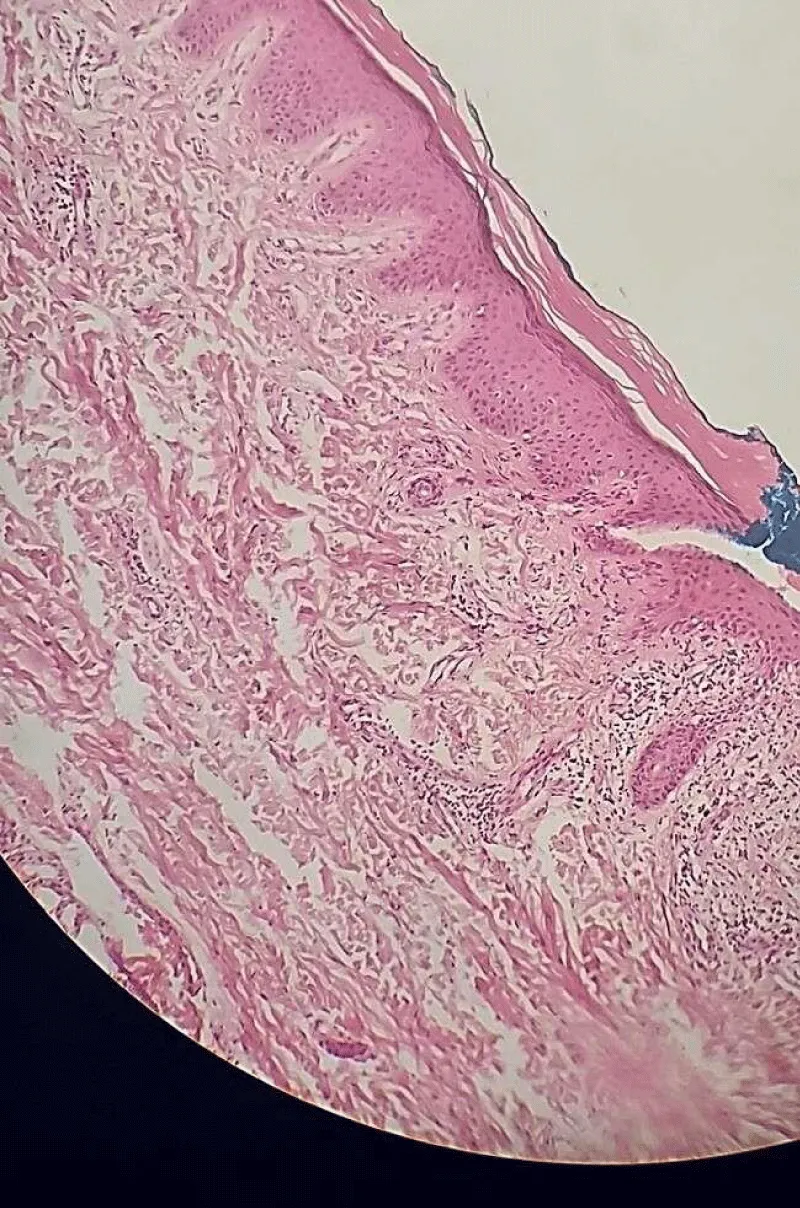
Laboratory investigations revealed hematologic investigations anemia and an elevated erythrocyte sedimentation rate. Biochemical tests for hepatic and renal functions, as well as chest radiograph were normal. Anti-nuclear antibodies (ANA) were positive. Whereas Anti SSA/RO-SSB/LA antibodies were negative. Complement levels (C3, C4) were low. Cryoglobulin testing was negative. Skin biopsy showed hyperkeratosis, degeneration of the basal area, fibrin deposition along the basement membrane, and a superficial and deep lymphocytic vascular reaction (Figure 2). These findings were compatible with the diagnosis of CHLE.
Figure 2: A-histological finding of CHLE: hyperkeratosis, degeneration of the basal area, fibrin deposition on the basement membrane, and a superficial and deep lymphocytic vascular reaction.
Our Treatment plan included cold protection in addition to topical corticosteroids twice daily, which led to significant improvement after two weeks (Figure 3).
Figure 3: A, B, C- All lesions almost cleared after two weeks of treatment.
Chilblain Lupus is an uncommon subtype of Cutaneous Lupus Erythematosus, occurring in both sporadic and inherited forms [2,3]. It is characterized by tender, pruritic red or dusky patches, papules, plaques, and nodules, which may sometimes show central erosion or ulceration. Lesions typically affect acral regions of the body that are most exposed to cold, such as the toes, fingers, ears, and other extremities [4-6]. CHLE is triggered by exposure to cold and moisture in a cool climate, which stimulates vascular thrombosis, blood stasis, and impaired microcirculation [3]. It is often associated with immunological markers, including antinuclear antibodies, rheumatoid factor, and anti-Ro \SSA antibodies [7]. Histopathological findings reveal a lymphocytic vascular reaction in both the superficial and deep layers of the skin, along with interface dermatitis. Direct immunofluorescence studies show linear deposits of IgM, IgA, or C3 at the dermal-epidermal junction [8,9]. The Differential diagnosis of chilblain lupus erythematosus includes perniosis, lupus pernio, Raynaud’s phenomenon, and livedo reticularis [6]. Differentiating CHLE from perniosis is particularly challenging due to overlapping clinical features. However, CHLE is more likely to be associated with systemic autoimmune markers and histological features of lupus. The ‘Mayo Clinic Diagnostic Criteria ‘for diagnosing chilblain lupus erythematosus are outlined in (Table 1) [10].
| Table 1: Diagnostic Criteria for Chilblain Lupus Erythematosus adapted from Mayo Clinic criteria [10]. |
| Major Criteria 1. Skin lesions located in acral areas induced by cold weather and aggravated by cold 2. Histopathology consistent with lupus erythematous. |
| Minor criteria 1. Coexistence of systemic or discoid lupus erythematosus 2. Response to anti-LE therapy. 3. Negative cryoglobulin and cold agglutinin studies. |
| Diagnosing a patient requires two major and at least one minor criterion |
In our case the patient fulfilled all the major and minor criteria, including acral distribution of the lesions, histopathological findings consistent with lupus erythematous, and the presence of a malar rash, as well as negative cold agglutinin test and improvement of the lesions with anti-Lupus Erythematosus therapy.
In general, the treatment of Chilblain Lupus Erythematosus includes the following approaches:
- Preventive Measures such as avoiding cold exposure and smoking cessation.
- Antibiotics used in cases of secondary bacterial skin infections.
- Topical treatments such as topical steroids and calcineurin inhibitors.
- Systemic treatments including calcium channel blockers to improve circulation, systemic corticosteroids and immunosuppressive agents like mycophenolate mofetil and antimalarial drugs [3,11-13].
Our patient applied topical corticosteroids twice daily in addition to cold protection measures. We noticed remarkable improvement after just two weeks of treatment. We proposed initiating calcium channel blockers during winter if the lesions become symptomatic. Since the risk for Systemic Lupus Erythematosus (SLE) in such cases is about 18%, regular follow-up every six months is recommended to monitor for evidence of progression to SLE.
To conclude, CHLE lesions could be challenging for clinicians, which is why they should always be bear in mind-especially in lesions that are triggered or aggravated by cold weather, therefore, thorough evaluations and appropriate investigations are essential in suspicious cases. Hence, early recognition and appropriate management can lead to excellent outcomes and may prevent progression to systemic disease.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Declarations
Ethical approval and consent to participate: Approval was obtained from the ethics committee of the Faculty of Medicine at Damascus University.
Ethics statement: Ethical approval was obtained from the ethics committee the Faculty of Medicine at Damascus University. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Data availability: All data generated or analyzed during this study are included in this published article.
Author contributions
Reem Hasan contributed to the diagnosed and follow up of the case and to writing the manuscript.
Nemat Alsaghir contributed to and supervised the diagnosis, follow-up, and manuscript preparation.
Seba Ibrahim contributed to the writing of the manuscript.
- Bansal S, Goel A. Chilblain lupus erythematosus in an adolescent girl. Indian Dermatol Online J. 2014;5(Suppl 1):S30-2. Available from: https://doi.org/10.4103/2229-5178.144522
- Lee-Kirsch MA, Chowdhury D, Harvey S, Gong M, Senenko L, Engel K, et al. A mutation in TREX1 that impairs susceptibility to granzyme A-mediated cell death underlies familial chilblain lupus. J Mol Med (Berl). 2007;85(5):531-7. Available from: https://doi.org/10.1007/s00109-007-0199-9
- Hedrich CM, Fiebig B, Hauck FH, Sallmann S, Hahn G, Pfeiffer C, et al. Chilblain lupus erythematosus--a review of literature. Clin Rheumatol. 2008;27(8):949-54. Epub 2008 Jun 10. Erratum in: Clin Rheumatol. 2008;27(10):1341. Lee-Kirsch, Min Ae [added]. Available from: https://doi.org/10.1007/s10067-008-0942-9
- Kuhn A, Sticherling M, Bonsmann G. Clinical manifestations of cutaneous lupus erythematosus. J Dtsch Dermatol Ges. 2007;5(12):1124-37. English, German. Available from: https://doi.org/10.1111/j.1610-0387.2007.06554.x
- Hutchinson J. Harveian Lectures on Lupus. Br Med J. 1888;1(1411):58-63. Available from: https://doi.org/10.1136/bmj.1.1411.58
- Arias-Santiago SA, Girón-Prieto MS, Callejas-Rubio JL, Fernández-Pugnaire MA, Ortego-Centeno N. Lupus pernio or chilblain lupus?: two different entities. Chest 2009; 136: 946–7. Available from: https://doi.org/10.1378/chest.09-1005
- Franceschini F, Calzavara-Pinton P, Quinzanini M, Cavazzana I, Bettoni L, Zane C, et al. Chilblain lupus erythematosus is associated with antibodies to SSA/Ro. Lupus. 1999;8(3):215-9. Available from: https://doi.org/10.1191/096120399678847632
- Dubey S, Joshi N, Stevenson O, Gordon C, Reynolds JA. Chilblains in immune-mediated inflammatory diseases: a review. Rheumatology (Oxford). 2022;61(12):4631-4642. Available from: https://doi.org/10.1093/rheumatology/keac231
- Canu D, Viallard JF, Lazaro E, Doutre MS. Association of chilblain lupus and anti-Ro/SSA and anti-La/SSB antibodies: a study of 30 cases. Int J Dermatol. 2021;60(12):e509-e511. Available from: https://doi.org/10.1111/ijd.15553
- Su WP, Perniciaro C, Rogers RS 3rd, White JW Jr. Chilblain lupus erythematosus (lupus pernio): clinical review of the Mayo Clinic experience and proposal of diagnostic criteria. Cutis. 1994;54(6):395-9. Available from: https://pubmed.ncbi.nlm.nih.gov/7867381/
- Chang AY, Werth VP. Treatment of cutaneous lupus. Curr Rheumatol Rep. 2011;13(4):300-7. Available from: https://doi.org/10.1007/s11926-011-0180-z
- Gouillon L, Debarbieux S, Berruyer M, Fabien N, Lega JC, Thomas L. Chilblain lupus erythematosus treated successfully with mycophenolate mofetil. Int J Dermatol. 2017;56(8):e158-e159. Available from: https://doi.org/10.1111/ijd.13614
- Cavazzana I, Sala R, Bazzani C, Ceribelli A, Zane C, Cattaneo R, et al. Treatment of lupus skin involvement with quinacrine and hydroxychloroquine. Lupus. 2009;18(8):735-9. Available from: https://doi.org/10.1177/0961203308101714