More Information
Submitted: June 15, 2023 | Approved: June 23, 2023 | Published: June 24, 2023
How to cite this article: Karabinta Y, Dissa L, Karambé T, Koné C, Diarra D. An Urticaria Closet Simulating Leprosy in A 36-Year-Old Woman. Ann Dermatol Res. 2023; 7: 016-017.
DOI: 10.29328/journal.adr.1001025
Copyright License: © 2023 Karabinta Y, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Urticaria; Closet; Leprosy
An Urticaria Closet Simulating Leprosy in A 36-Year-Old Woman
Yamoussa Karabinta1,2*, Labassou Dissa1, Ténin Karambé3, Chaka Koné1 and Diaratou Diarra1
1Dermatology Teaching Hospital of Bamako, Mali
2Medical and Dental Faculty of Bamako, Mali
3Teaching Hospital of Gabriel TOURE, Bamako, Mali
*Address for Correspondence: Dr. Karabinta Yamoussa, Assistant Professor, FMOS/USTTB, BP: 251, Bamako, Mali, Email: [email protected]
Urticaria corresponds to a papular edematous pruriginous fleeting rash on the skin whose cause is most often allergic (food, medicines, insect bites, etc.).
Its management is often difficult because of its significant impact on quality of life. Its prevalence is estimated at 0.6% - 1.3% of the general population. Leprosy is a chronic infectious disease caused by Mycobacterium leprae (M. leprae) or Hansen’s bacillus (BH). Considered as the great simulator leprosy can pose a diagnostic problem with many other dermatological pathologies. This is a 36-year-old patient with a history of chronic urticaria treated with Loratadine 10 mg who consulted the Bamako Dermatology Hospital for a large erythematous cupboard, oedematous fixed on the buttocks evolving for more than 3 days. The interrogation found the notion of pruritus, hives, and physical examination, showed large erythematous plaques, edematous very limited, dark red color, and slightly copper resembling the closet infiltrated by leprosy. The pruriginous nature of the lesions and the absence of other cardinal signs of leprosy allowed us to make the diagnosis of chronic urticaria.
Urticaria is a fleeting itchy papular rash on the skin, the cause of which is most often allergic (food, medicines, insect bites, etc.) [1]. It can be acute for less than 6 weeks or chronic for more than 6 consecutive weeks [1]. Its management is often difficult because of its significant impact on quality of life, its potential association with many underlying pathologies, and sometimes an inadequate response to first-line treatment [1,2]. Its prevalence is estimated at 0.6% - 1.3% of the general population [2]. Several causes can induce physical hives such as cold, heat, and pressure [3]. Leprosy is a chronic infectious disease caused by Mycobacterium leprae (M. leprae) or Hansen’s Bacillus (BH) [4]. Its prevalence is estimated at about 200,000 new cases annually worldwide [5]. It is the first infectious cause of nerve damage and infirmity in developing countries [5]. Considered the great simulant leprosy can pose a diagnostic problem with many other dermatological pathologies including urticaria. We reported a case of urticaria closet resembling leprosy in a 36-year-old patient.
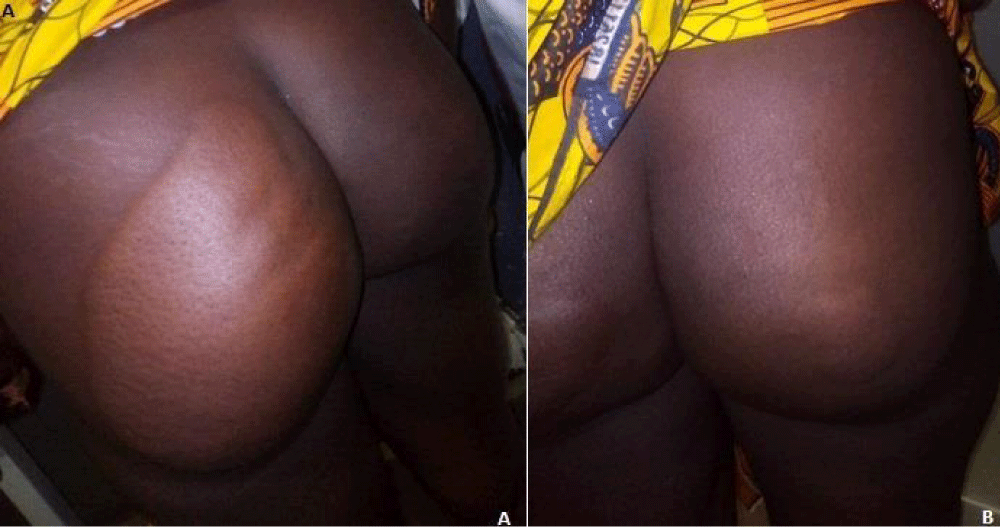
This is a 36-year-old patient with a history of chronic urticaria treated with Loratadine 10mg due to one tablet per day. She consulted on April 25, 2023, at the dermatology hospital in Bamako for a large erythematous cupboard, oedematous fixed on the buttocks evolving for more than 3 days. The onset of the symptomatology was 2 weeks old and was marked by the appearance of multiple itchy erythematous papules on the trunk and upper limbs. In front of this symptomatology, she consults with her doctor in a health center of the place who made the diagnosis of urticaria and prescribed Desloratadine 5 mg, 2 tablets per day associated with an emollient that leads to remission of lesions and improvement of pruritus. A few weeks later, 2 large erythematous and edematous closets appear on her buttocks (Figures 1A,1B). This motivated a consultation with her doctor who referred her to the University Dermatology Hospital for treatment. The interrogation returned to the notion of pruritus, hives. On physical examination, we found the presence of large erythematous plaques, oedematous very limited, dark red color, and slightly copper resembling the infiltrated cupboard of leprosy. These plates converge in large cupboards, the largest of which measures 25 cm/20 cm (Figure 1A) and the smallest 4 cm/3 cm (Figure 1B) located on both buttocks. The surface of these lesions is smooth. On palpation, the peripheral nerves (ulnar and radial, femoral, external popliteal) were not sensitive or hypertrophied. The muscular strength of the limbs was retained.
Figure 1: A) Confluent edematous papules in the cupboard; B) Multiple edematous papules on buttocks.
The palms of the hands and soles of the feet were not hypoesthesia. There is no dermatographism sign detected on the physical examination. However, there were any associated symptoms such as flu-like symptoms, fever, fatigue, and arthralgia. The bacilloscopic examination was normal as well as the histology of a skin biopsy fragment. A completed blood count resulted in polynuclear predominant leukocytosis. the results of the biological examination show: Red blood cells (4,37x1012/l), Hemoglobun (13,5g/dl), Leucocyte (4100/mm3), Leukocyte formula: Neutrophils (43,6%), eosinophilic polynuclear cells (7,9), Basophilic polynuclear (3,5), T Cell (42,0), Circulatory Monocyte (10.0), Sedimentation rate (first hour: 7 mm, Second hour: 29 mm), C-reactive protein (low than 3.00 mg/l), Blood glucose (4,27 mmol/l, Creatine (0,85 mg/dl), Transaminase (ALT:13UI/l, AST: 10UI/l).
The examination of the biopsy part showed dermal edema, inflammatory infiltrate, capillary dilations, and perivascular, composed of eosinophilic polynuclear and neutrophil polynuclear.
This clinical observation involved a case of chronic urticaria of atypical presentation incompatible with the typical form which made us think of lepromatous leprosy. The etiologies of chronic urticaria are multiple and sometimes entangled, making the etiological approach difficult and disappointing [6,7]. In our patient, these skin lesions evoke copper erythematous cupboards characteristic of Hansen’s disease. However, the other cardinal signs allowing the diagnosis of leprosy were absent in our patient (peripheral nerve hypertrophy, Bacilloscopy histology, and presence of BAAR), but it was appropriate to think of leprosy in an area of the endemic leper in front of these bright red erythematous cupboards. Leprosy presents a lesional polymorphism that can be confusing with many dermatological pathologies. The epidemiological characteristics of leprosy, and more particularly the distribution of the various clinical forms, vary significantly across continents [6]. The WHO encourages national leprosy control programs to mass screen for new cases of leprosy for eradication. This motivated us to think and look for signs of leprosy. The examination and physical examination were contributory to the diagnosis. Various causes can induce physical hives such as cold, heat, and pressure. We believe that the pressure of the buttocks on the chairs due to prolonged sitting would be the cause of these physical hives in our patient who is a secretary. There are several sites of pressure urticaria. in addition to buttocks, pressure urticaria can sit on the back in supportives, on the thighs.
Although urticaria is an easy-to-diagnose pathology, it is essential to rule out other dermatoses due to its atypical presentation. One of these dermatological pathology to be ruled out is Hansen’s disease which is a great simulator. So in front of any infiltrated erythematous closet, it is essential to eliminate leprosy early to avoid a fatal evolution of the disease.
Ethical considerations: The patient’s free and lighted consent was obtained for the publication of his photo.
- Staumont-Sallé D, Piette F, Delaporte E. Bilan étiologique et traitement d'une urticaire chronique [Etiological diagnosis and treatment of chronic urticaria]. Rev Med Interne. 2003 Jan;24(1):34-44. French. doi: 10.1016/s0248-8663(02)00003-6. PMID: 12614856.
- Morel V, Hauser C. Urticaire chronique [Chronic urticaria]. Rev Med Suisse. 2008 Apr 23;4(154):1019-23. French. PMID: 18557530.
- Aracting S. Formes cliniques de l’urticaire chronique chez l’adulte. Rev Franc Allerg. 2003; 44(1):103-107.
- Traoré B, Cissé L, Fofana Y, Coulibaly A, Somboro D, Gassama M. Carcinome épidermoide sur ulcération d’origine lépreuse. Bull de l’Allf. 2018; 33:8-10.
- Fall L, Guèye AB, Ndoye GF, Kinkpé CVA, Chaise F. Neuritis of the deep fibular/anterior tibial nerve of leprous origin in a case observed at the hospital center of the order of malta in dakar, senegal. Allf Bull, 2018; 33:11-14.
- Millan J. Anthropogenetic approach of a Hansenian population in Guadeloupe. Allf Bull, 2018; 33 :22-25.
- Bouassaid R. Prise en charge de l’urticaire chronique dans les pays du Magreb. Rev Fran Aller. 2016; 56(3):293.