More Information
Submitted: March 15, 2023 | Approved: April 04, 2023 | Published: April 05, 2023
How to cite this article: Potekaev NN, Sysoeva VS, Bobko SI, Katunina OR, Borodulina KS. Subcorneal pustular dermatosis (Sneddon-Wilkinson disease): a case report. Case reports. Ann Dermatol Res. 2023; 7: 013-015.
DOI: 10.29328/journal.adr.1001024
Copyright License: © 2023 Potekaev NN, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Subcorneal pustular dermatosis; Sneddon-Wilkinson disease; Path morphology; Dapsone; Phototherapy
Subcorneal pustular dermatosis (Sneddon-Wilkinson disease): a case report
Potekaev NN1,2 , Sysoeva VS1
, Sysoeva VS1 , Bobko SI1*
, Bobko SI1* , Katunina OR1
, Katunina OR1 and Borodulina KS1
and Borodulina KS1
1Moscow Scientific and Practical Center of Dermatovenerology and Cosmetology, Moscow, 119071, Russia
2N.I. Pirogov Russian National Research Medical University, Moscow, Russia, 117321
*Address for Correspondence: Bobko SI, Moscow Scientific and Practical Center of Dermatovenerology and Cosmetology, Moscow, 119071, Russia, Email: [email protected]
This article contains modern data on the etiology, clinical presentation and treatment as well as the differential diagnosis of a rare dermatosis, Sneddon-Wilkinson disease.
Clinical observation of subcorneal pustular dermatosis in a 68-year-old woman is reported. Histopathological examination played a key role in making the correct diagnosis. Treatment consisted of a physiotherapeutic approach (311 nm UVB phototherapy) in combination with systemic glucocorticosteroids (dexamethasone). This therapeutic approach (instead of dapsone therapy) can be used due to its relatively good safety profile.
Subcorneal pustular dermatosis or Sneddon-Wilkinson disease (SPD) is a rare chronic benign relapsing vesiculo-pustular disease of unknown ethiology, that most commonly occurs in middle-aged and elderly women. At the same time, rare cases of the development of SPD in children are described in the literature [1].
Although the cause of occurrence remains unknown, the role of previous or concomitant infections cannot be ruled out [2]. Endocrine disorders, mental disturbances, and immunoallergic diseases have a certain value in the occurrence of the disease [3]. In addition, there is a number of diseases associated with subcorneal pustulosis, such as monoclonal gammopathy, multiple myeloma, rheumatoid arthritis, Crohn’s disease, pyoderma gangrenosum, Sweet syndrome, Crocker-Williams persistently elevated erythemа, pustular psoriasis, SAPHO syndrome (synovitis, acne, gangrenous pyoderma, osteitis). There are reports on the relationship of SPD with aplastic anemia, mycoplasmal pneumonia, cystic lesions of the liver in some helminthiasis, hyperthyroidism, and thymoma [4,5]. Pregnancy can be also a precipitating factor [6].
On normal or more often slightly erythematous skin primary focus of the disease appear in groups – small (up to 5 mm in diameter). Superficial pustules with a flabby tire contain neutrophils. The lesions are prone to confluence and peripheral growth can form annular, serpiginous patterns. After opening they dry out and form superficial scale crusts resembling impetigo. In their place, slight hyperpigmentation may remain. Lesions are usually symmetrical, located mainly in large folds (axillary, inguinalfenoral), in the abdomen, under the mammary glands, and on the extensor areas of the limbs. Rarely, the face, palms, and soles are affected. Mucous membranes and skin of the scalp are always free from lesions. Subjectively patients may complain of a feeling of itching and burning, while the general condition remains satisfactory. Clinical and biochemical blood tests – no pathology [2,7]. Although the protein electrophoresis is carried out abroad because of the association of paraproteinemia with SPD [3] According to G. Baeza-Hernández, 2021, the etiological factor Mycoplasma Pneumoniae was discussed [8].
Histologically the main symptom of the disease is subcorneal pustules with polymorphonuclear leukocytes. The epidermal layer under the pustule has practical changes. In the dermis, a perivascular infiltrate containing neutrophils, single monocytes, and eosinophils is detected. Acantholysis is absent [2].
In a group of patients during a direct immunofluorescence reaction (RIF) sometimes deposits of IgA are found in the epidermis. In isolated cases, the method of indirect FIR reveals circulating antibodies to IgA directed against epidermal cells. According to the modern classification, such cases are described as the SPD type of pemphigus [9].
Differential diagnosis is presented in the Table 1.
Without treatment periods of exacerbation repeat for several years, while the duration of remissions varies from several days to several weeks. The drugs of choice are sulfones (predominantly dapsone) [10], in the treatment of which most often a complete remission is achieved. Acitretinmaybeasecond-line drug. The literature describes isolated cases of successful use of drugs such as colchicine, cyclosporine, infliximab, etanercept, tumor necrosis factor alpha blockers, maxacalcitol, mizoribine, ketoconazole, tetracycline, minocycline, benzylpenicillin, vitamin E, azithromycin [11], doxycycline [8,12], adalimumab [13]. The efficacy of systemic and topical glucocorticosteroids in elderly patients has also been reported [14,15].
Patient G., born in 1954, came to an outpatient appointment with complaints of lesions of the skin of the trunk, and upper and lower extremities, accompanied by periodic itching of moderate intensity. She was ill since 1988 when she first noted the appearance of lesions on the skin of the trunk after a seven-day fast. She independently used sulfuric ointment, according to the words, a skin biopsy was performed, but the diagnosis was not established (medical documents were not provided). Further notes of the undulating course of the process with periods of exacerbations and remissions, improvements against the background of insolation. Since 1992 she noted the spread of the process, hospitalization was carried out in a hospital, where the differential diagnosis was carried out between the diagnoses of Duhring dermatitis herpetiform and Subcorneal pustulosis, received treatment with a suspension for the external use of cindol and plasmapheresis. She was discharged with improvement. After suffering stress in 2017-2018 she noted another exacerbation of the process, phototherapy (UVB 311 nm) was carried out with a positive effect.
In 2022 due to another exacerbation, hospitalization in a daily stay hospital of the branch Clinic named after V.G. Korolenko for pathomorphological examination and in case of confirmation of the diagnosis of Sneddon-Wilkinson’s subcorneal pustulosis, the start of dapsone therapy. During the additional examination, she underwent a course of phototherapy with UVB 311 nm (14 sessions) with a temporary positive effect. She also received 5 injections of Hemodez solution, received Phosphogliv, Mexidol, dexamethasone solution 4 and 8 mg intramuscularly according to the recommendation of a polyclinic doctor - with a temporary positive effect, and the course of phototherapy was interrupted. External treatment was not carried out. She refused to take dapsone due to the improvement of the skin process.
Concomitant diseases: duodenal ulcer, nodular goiter. Bad habits are denied. Allergy anamnesis: allergic reaction to novocaine. Heredity: parents – diabetes mellitus, father – Parkinson's disease, brother – cancer of the kidney, thyroid cancer. Sexually transmitted infections, HIV, viral hepatitis, and tuberculosis denies. No blood transfusions. The patient fulfilled the special information form that allowed them to perform all the necessary consultations and examinations.
Objectively. The general condition is satisfactory
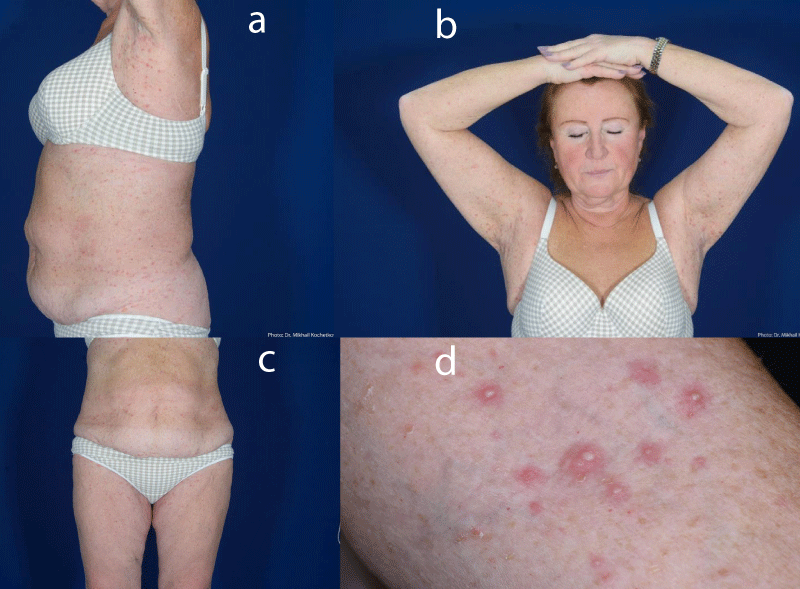
Local status: The pathological process on the skin is subacute, widespread, localized on the skin of the trunk, and symmetrically on the skin of the upper and lower extremities. Represented by papules, pustules with a flaccid tire, surrounded by an inflammatory corolla along the periphery, up to 0.5 cm in size, red, Nikolsky’s symptom is negative. There are no dermoscopic findings for atypia. Mucous membranes, the skin of the scalp, palms, and soles are intact (Figure 1a-d).
Figure 1: Rashes on the skin of the chest (1a), abdomen areas (1c), and arms (1b,d).
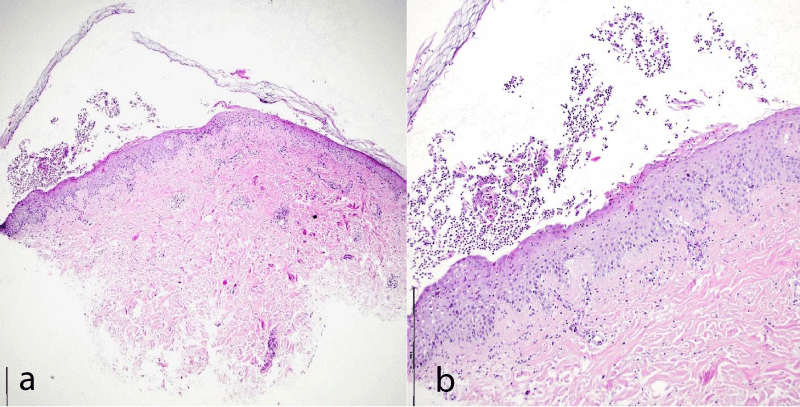
Data from laboratory examinations: Complete blood counts blood sedimentation rate 63 mm/h. Biochemical blood test: glucose 5.86, Rapid plasma reagin - negative, HBsAg negative, D-dimer more than 5000, glycosylated hemoglobin 6.2 Histological examination of a skin biopsy sample mild acanthosis of the epidermis with exocytosis of neutrophilic granulocytes into the epidermis, the presence of subcorneal pustules containing neutrophilic leukocytes, in some places single foci of spongiosis, single acantholytic cells are found. Around the vessels of the superficial plexus, there is a moderate lymphomonocytic infiltration with an admixture of neutrophilic granulocytes, leukocyte stasis is present in the lumen of the vessels (Figure 2a,b).
Figure 2: The pathomorphological pattern of the skin biopsy specimen.
Conclusion: Pathomorphological changes can be observed in Sneddon-Wilkinson subcorneal pustulosis, clinically differentiated from superficial pyoderma (bullous impetigo). Based on the clinical picture and histological examination data, the diagnosis was made Sneddon-Wilkinson subcorneal dermatosis.
H&E staining with different magnifications.
The presented clinical case has high interest from the point of view of the complexity of the differential diagnosis of the rare Sneddon-Wilkinson dermatosis. To prescribe adequate therapy, only a pathomorphological study will help dermtovenereologists to confirm the correct diagnosis. In addition, this case demonstrates the effectiveness of physiotherapy (311 nm UVB phototherapy) in combination with systemic glucocorticosteroids (dexamethasone).
This approach may be advantageous in patients with contraindications to dapsone therapy or with severe comorbidities in the treatment of subcorneal pustulosis due to a lower likelihood of side effects.
- Alhafi MA, Janahi MI, Almossalli ZN. Subcorneal Pustular Dermatosis in Paediatrics: A Case Report and Review of the Literature. Cureus. 2021 Dec 6;13(12):e20221. doi: 10.7759/cureus.20221. PMID: 35004040; PMCID: PMC8729309.
- Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, Orringer JS. Fitzpatrick’s Dermatology 9th Eighth Edition. 2019.
- Askhakov MS, Chebotarev VV, Odinets AV. Dermatosis subcorneal pustular Sneddon-Wilkinson. Medical Bulletin of the North Caucasus. 2015;10:1:107-109. https://doi.org/10.14300 / mnnc 2015.10023
- Drozhdina MB, Koshkin SV. Sneddon - Wilkinson disease: Review of the modern literature. Bulletin of Dermatology and Venereology. 2019; 95:15-20. https://doi.org/10.25208/0042-4609-2019-95-1-15-20
- Ferrillo M, Villani A, Fabbrocini G, Mascolo M, Megna M, Costa C, Napolitano M. A Case of the Co-Existence of Subcorneal Pustular Dermatosis and Pyoderma Gangrenosum and a Review of the Literature. Open Access Maced J Med Sci. 2018 Jul 8;6(7):1271-1274. doi: 10.3889/oamjms.2018.214. PMID: 30087735; PMCID: PMC6062289.
- Bhargava S, Kumar U, Kroumpouzos G. Subcorneal pustular dermatosis: Comprehensive review and report of a case presenting during pregnancy. Int J Womens Dermatol. 2020 Feb 20;6(3):131-136. doi: 10.1016/j.ijwd.2020.02.003. Erratum in: Int J Womens Dermatol. 2021 Sep 28;7(5Part B):867. PMID: 32637535; PMCID: PMC7330443.
- Karacheva YV, Smykova AN. Subcorneal pustular dermatosis of Sneddon-Wilkinson: Сlinical case. Russian Journal of Skin and Venereal Diseases. 2018; 21: 28-30. https://doi.org/10.18821/1560-9588-2018-21-1-28-30
- Baeza-Hernández G, Guerrero-Torija A, Rubio-Aguilera RF, Khedaoui R, Martínez-Morán C, Borbujo J. Mycoplasma Pneumoniae-associated Subcorneal Pustular Dermatosis: Not as Rare as We Think? Dermatol Pract Concept. 2022 Oct 1;12(4):e2022168. doi: 10.5826/dpc.1204a168. PMID: 36534515; PMCID: PMC9681174.
- Raznatovskiĭ KI, Piriatinskaia VA, Kariakina LA, Smirnova ON, Lalaeva AM, Vinnichuk SA, Khabbus AG. Pustular dermatosis (Sneddon—Wilkinson disease): case study. Clinical Dermatology and Venereology. 2017; 16(3):36‑40. https://doi.org/10.17116/klinderma201716336-39
- Ghatnekar S, Rutherford A, Vandergriff T, Yancey KB. Dapsone-responsive inflammatory dermatitis with features of subcorneal pustular dermatosis and bullous pemphigoid. JAAD Case Rep. 2022 Feb 3;24:29-31. doi: 10.1016/j.jdcr.2022.01.026. PMID: 35572198; PMCID: PMC9098384.
- Watts PJ, Khachemoune A. Subcorneal Pustular Dermatosis: A Review of 30 Years of Progress. Am J Clin Dermatol. 2016 Dec;17(6):653-671. doi: 10.1007/s40257-016-0202-8. PMID: 27349653.
- Borgia F, Campitiello A, Di Bartolomeo L, Cardia R, Marafioti I, Cannavò SP. Subcorneal pustular dermatosis successfully treated with low-dose doxycycline. Int J Dermatol. 2021 Sep;60(9):e375-e376. doi: 10.1111/ijd.15530. Epub 2021 Apr 16. PMID: 33860941.
- Chen J, Luo Y, Yu N, Yang Y, Zhou X, Zhang S, Ye Q, Zhu H. Successful Treatment of Severe Subcorneal Pustular Dermatosis with Adalimumab. Clin Cosmet Investig Dermatol. 2022 Nov 28;15:2567-2570. doi: 10.2147/CCID.S391594. PMID: 36466943; PMCID: PMC9717427.
- Ceccarelli G, Molinelli E, Campanati A, Goteri G, Offidani A. Sneddon-Wilkinson Disease and Monoclonal Gammopathy of Undetermined Significance in the Elderly: Case Report. Case Rep Dermatol. 2019 Jul 10;11(2):209-214. doi: 10.1159/000487003. PMID: 31427943; PMCID: PMC6696771.
- Hashimoto T, Teye K, Ishii N. Clinical and immunological studies of 49 cases of various types of intercellular IgA dermatosis and 13 cases of classical subcorneal pustular dermatosis examined at Kurume University. Br J Dermatol. 2017 Jan;176(1):168-175. doi: 10.1111/bjd.14780. Epub 2016 Oct 17. PMID: 27258999.