More Information
Submitted: April 27, 2021 | Approved: April 29, 2021 | Published: April 30, 2021
How to cite this article: Torres-Gómez FJ. 58-year-old male patient who came to the dermatology service for a clinical picture. Ann Dermatol Res. 2021; 5: 018-019.
DOI: 10.29328/journal.adr.1001016
Copyright License: © 2021 Torres-Gómez FJ. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
58-year-old male patient who came to the dermatology service for a clinical picture
Francisco Javier Torres-Gómez*
High Resolution Hospital, Utrera, Sevilla, Spain
*Address for Correspondence: Francisco Javier Torres-Gómez, High Resolution Hospital, Avda Brigadas Internacinales s/n. 41710 Utrera, Sevilla, Spain, Tel:34+629344869; Email: [email protected]
58-year-old male patient who came to the dermatology service for a clinical picture consisting of generalized erythematous scaly and pruritic lesions of 2 years of evolution. The clinical judgments provided were: pityriasis versicolor, drop psoriasis, pityriasis rubra pilaris and secondary syphilis (without serology confirming this last hypothesis then). A biopsy of a lesion located on the right costal side was performed. The serology was negative in a second time.
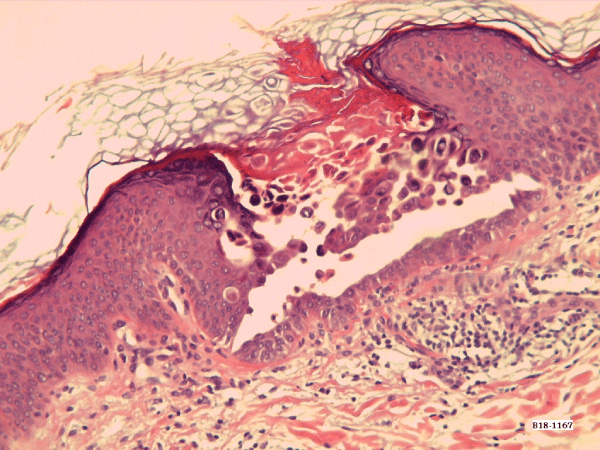
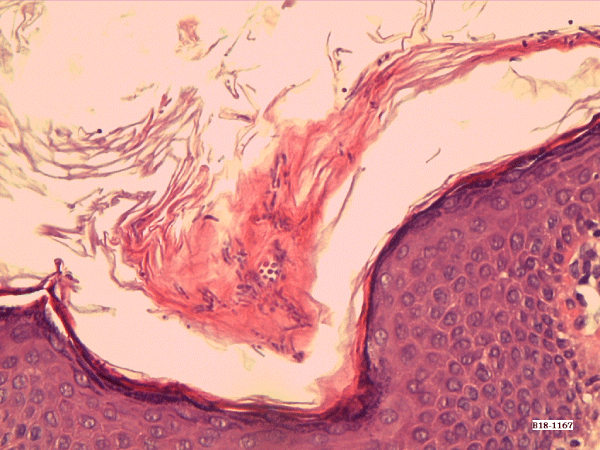
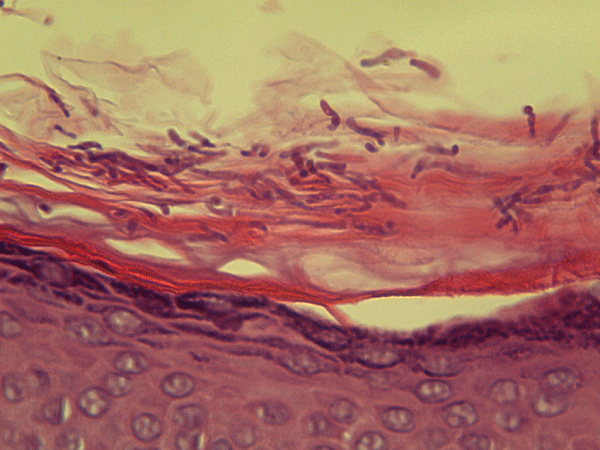
Histologically, an isolated focus of epidermal acantholysis was observed, associated with a corneal layer with a basket pattern that was preserved but detached. The presence of fungal hyphae (PAS +) in superficial and corneal epidermal strata was confirmed. At the superficial dermis level, only a discrete lymphocytic inflammatory infiltrate was observed in relation to the acantholysis focus. Systemic antifungal treatment resolved the condition.
There were no infiltrative neutrophil polymorphonuclear leukocytes or epidermal hyperplasia characteristic of psoriasis, plasmacytic infiltrate neither vascular changes characteristic of syphilis, or folliculotrophism and parakeratosis typical of pityriasis rubra pilaris.
Was our case a case of pythiasis versicolor? Pityriasis versicolor (tinea versicolor) is a superficial fungal condition typical of tropical climates with manifestations and exacerbations in warm months, more frequent in n young patients (mean age 20-40 years) and a predilection for the female sex. Our patient was an older male, caucasian, living in Andalusia, in southern Spain, and the condition was identified in the autumn.
Tinea versicolor lesions tend to have a preference for seborrheic and moist areas, unlike our patient, in whom the generalized lesions did not coincide with folds or seborrheic areas. The popular and non-macular lesions showed superficial scales of very small size but no pigmentation, all of which were not consistent with ringworm. The absence of follicular changes, parakeratosis, pigmentation and melanophages make us doubt the diagnosis of pityriasis versicolor, although we admit that we could be facing an acantholytic variant of it. Systemic antifungal treatment was effective and the clinical picture resolved completely [1,2] (Figures 1-3).
Figure 1: Focal acantholysis without concomitant inflammatory infiltrate. Round keratinocytes and preservation of the epidermal stratum basalis can be observed. HE 100x.
Figure 2: Fungal spores and hyphae interspersed with keratin scales on the epithelial surface. HE 200x.
Figure 3: Detail of fungal hyphae. PAS 400x.
- Varada S, Dabade T, Loo DS. Uncommon presentations of tinea versicolor. Dermatol Pract Concept. 2014; 4: 93-96. PubMed: https://pubmed.ncbi.nlm.nih.gov/25126470/
- Ferry M, Shedlofsky L, Newman A, Mengesha Y, Blumetti B. Tinea InVersicolor: A Rare Distribution of a Common Eruption. Cureus. 2020; 12: e6689. PubMed: https://pubmed.ncbi.nlm.nih.gov/32104626/