More Information
Submitted: April 19, 2021 | Approved: April 27, 2021 | Published: April 28, 2021
How to cite this article: Karabinta Y, Gassama M, Gassama AH, Dicko A, Sanogo H, et al. Drug Eruptions at Patients in Consultation at the Dermatology Department of the Dermatology Teaching Hospital in Bamako, Mali: Epidemiological, Clinical and Etiological Study. Ann Dermatol Res. 2021; 5: 013-017.
DOI: 10.29328/journal.adr.1001015
ORCiD: orcid.org/0000-0001-7872-7937
Copyright License: © 2021 Karabinta Y, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Drug Eruptions at Patients in Consultation at the Dermatology Department of the Dermatology Teaching Hospital in Bamako, Mali: Epidemiological, Clinical and Etiological Study
Yamoussa Karabinta1,2*, Mamadou Gassama1,2, Aboubakar Hemedi Gassama1, Adama Dicko1,2, Hawa Sanogo5, Karambe Tenin1, Chata Traoré1, Mamourou Diakité1, Chaka Koné1, Sounkalo Dao3, Yannick Mukendi1, Moussa Savané4 and Faye Ousmane Faye1,2
1Dermatology Teaching Hospital of Bamako, Mali
2Faculty of Medicine and Dentistry of Bamako, Mali
3Infectious and Tropical Diseases Department, Teaching Hospital of Point G, Bamako, Mali
4Dermatology Department of Teaching Hospital of Gabriel TOURE, Bamako, Mali
5Reference Health Center of III, Bamako, Mali
*Address for Correspondence: Dr. Yamoussa Karabinta, Assistant Professor, FMOS/USTTB, BP: 251, Bamako, Mali, Tel: (+223) 76014532; Email: [email protected]
The administration of a drug substance is an essential step in the management of a patient. It aims either to cure the patient, to prevent a given disease or sometimes to help with the diagnosis. Unfortunately, the action of the drug can go beyond the desired effect, and cause skin-mucous accidents. These accidents, also known as drug-induced attacks, can be isolated or associated with systemic manifestations [1]. Drug eruption is a real public health issue because of the high frequency. In Europe, drug eruption is responsible for about 20% of spontaneous reports of drug accidents. They complicate 2% to 3% of hospital treatments and motivate 1% of consultations, 5% of hospitalizations in dermatology [2]. Some African authors were interested in the subject. Reported prevalence in hospital settings ranges from 0.4% to 1.53% [3,4]. In Mali, there are no national figures. Old statistics from the Department of Dermatology show that about thirty cases occur each year, most of which are represented by severe forms. However, the risk of drug eruption is thought to be very high due to increased local use of drugs without medical advice, the illegal proliferation of drug outlets (‘Street Medicine’). And the lack of enforcement of existing regulations. In addition, some authors believe that the advent of antiretrovirals and the use of antiInfectious infections used to treat opportunistic infections have increased the risk of Drug eruption by 4 to 30 times, particularly in subjects infected with the acquired human immunodeficiency virus (HIV) [2]. This same risk can be observed in leprosy patients on combination chimotherapy. Clinically, the diagnosis of drug eruption is not as easy as one might think because of clinical polymorphism. The responsibility of a drug for the onset of a reaction is also not easy to establish, as in most cases several drugs are administered simultaneously before the onset of the rash. Because of illiteracy, patients find it difficult to make a complete list of the molecules consumed. To this must be added the high frequency of counterfeit medicines circulating both on the street and in private pharmacies. Given the scarcity of African studies and due to local specificities, it seemed interesting to us to undertake a study on Drug eruption in the dermatology department of the Dermatology teaching hospital of Bamako whose purpose is to study epidemiological aspects, clinical, etiological and to identify the molecules responsible in these patients.
The dermatology department of the Dermatology Teaching Hospital served as a framework for our study. The Dermatology Teaching Hospital is a public scientific and technological institution (EPST). Its activity centre covers research on endemic diseases, vaccine research, clinical research, programme support, continuing education and teaching. It is located in 6th arrondissement of the district of Bamako precisely in the neighborhood of djicoroni para. This is a descriptive cross-sectional survey of all new patients consulting in the Dermatology Teaching hospital from 01 January 2019 to 31 December 2020. The study population consisted of consulting patients in the dermatology department during the study period.
The case was defined as any patient, regardless of age and sex, for a skin rash due to oral administration of a molecule. The imputability criteria used to search for the drug probably in question were those recommended by the French pharmacovigilance [5].
This was a systematic sampling to include all cases of toxiderma over a 2-year period in a specialized centre. We have included all patients consulted in the dermatology department of the Dermatology teaching hospital of Bamako and having the following characteristics: Rash compatible with a clinical presentation of toxidermis, appearance in the aftermath of the administration of a drug, agreeing to participate in the study. We systematically excluded: Autoimmune bullous diseases, too long time between eruption and administration of the molecule. All patients included were thoroughly interviewed. Socio-demographic data were collected on a survey sheet (Appendix). The chronological list of all recently taken medications (4 weeks prior) was carefully noted (molecule, dosages, reason for taking, duration, start and end of use). The notion of the occurrence of a similar episode was also sought. All patients were subjected to a complete dermatological examination. Retroviral serology was also prescribed.
TZANCK cytodiagnosis and skin biopsy were performed in the event of a new bubble. Stevens Johnson Syndrome and toxic epidermal necrolysis were routinely hospitalized. The informed consent of each patient was obtained before its inclusion. The iconography scrupulously respects the anonymity of the patients.
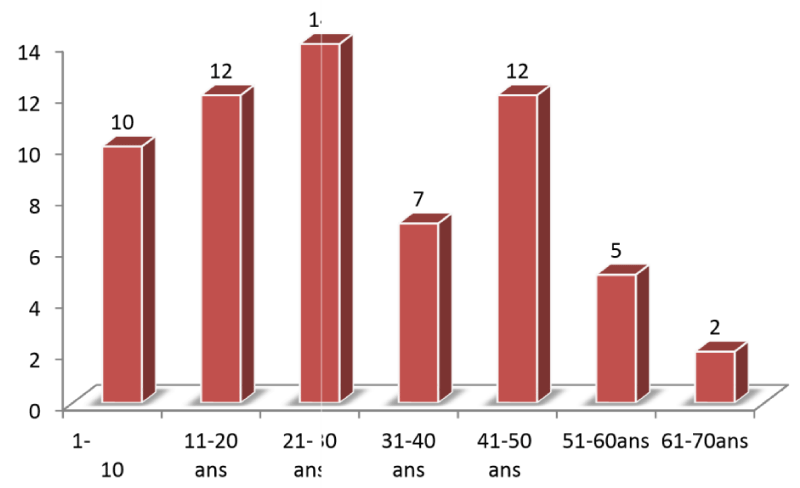
In total, during the study period 62 consultant cases for toxidermis were included in a sample of 2,129 patients, a prevalence of 2.91%. There were as many men (31 cases, 50%) as women, a sex ratio equal to 1 (Figures 1,2) (Table 1).
Figure 1: Gender disttibution.
Figure 2: Age group distribution.
| Table 1: Ethnic group distribution. | ||
| Ethnic | Frequency | Percentage |
| Peulh | 14 | 22,6% |
| Bambara | 13 | 21% |
| Soninke | 9 | 14,5% |
| Senoufo | 2 | 3,2% |
| Sonrhaï | 2 | 3,2% |
| Bozo | 1 | 1,6% |
| Dogon | 1 | 1,6% |
| Minianka | 1 | 1,6% |
| Autres | 19 | 30,6% |
| Total | 32 | 100% |
Patients came mainly from the regions of Bamako (71%), Koulikoro (14.5%), Sikasso (6.4%) and Ségou (4.8%) (Table 2).
| Table 2: Distribution by place. | ||
| Number | Frequency | Percentage |
| Bamako | 44 | 71% |
| Kayes | 1 | 1,6% |
| Koulikoro | 9 | 14,5% |
| Ségou | 3 | 4,8% |
| Sikasso | 4 | 6,5% |
| Autres | 1 | 1,6% |
| Total | 62 | 100% |
Clinically, only 3.2% of patients had a history of atopy (Table 3).
| Table 3: Distribution of patients accordant to the concept of drug allergy. | ||
| drug allergy | frequency | Percentage |
| Allergic | 7 | 11,3% |
| No allergic | 55 | 88,7% |
| Total | 62 | 100% |
Conditions that led to drug use: Approximately one-third of patients (31.5%, 22 cases) became acutely ill as a result of drug use for malaria or suspected malaria fever. For the rest, toxidermis occurred in the course of treatment for rhino-bronchitis (7 cases), angina (4 cases), gout (4 cases), epilepsy (3 cases) and headache (3 cases), leprosy (1 case), HIV and HIV-related opportunists (2 cases) (Table 4).
| Table 4: Distribution by reason of drug used. | ||
| Reason of drug used | Frequency | Percentage |
| Angina | 4 | 6,5% |
| Malaria | 22 | 31,5% |
| Rhinobronchitis | 7 | 11,3% |
| Gout | 4 | 6,5% |
| Epilepsy | 3 | 4,8% |
| Headache | 3 | 4,8% |
| HIV | 2 | 3,2% |
| Fever | 2 | 3,2% |
| Anemia | 1 | 1,6% |
| Cancer | 2 | 3,2% |
| Lupus | 1 | 1,6% |
| Parasitosis | 1 | 1,6% |
| IST | 1 | 1,6% |
| Sexial disoder | 1 | 1,6% |
| Gastralgia | 1 | 1,6% |
| Diarrhea | 11 | 1,6% |
| Paraplégia | 11 | 1,6% |
| Leprosis | 1 | 1,6% |
| Nephrotic Colic | 1 | 1,6% |
| No found | 1 | 1,6% |
| Preventive | 2 | 3,2% |
| Total | 62 | 100% |
Number of drugs consumed: The number of drugs consumed per patient ranged from 1 to 5 drugs, with an average of 1.8 1.6. Note that all had received at least one molecule (Tables 5,6).
| Table 5: Distribution by number of drugs kaked. | ||
| Number de médicament | Frequence | Percentage |
| One Drug | 22 | 35,5% |
| Two Drugs | 28 | 45,2% |
| Three Drugs | 10 | 16,1% |
| Four Drugs | 1 | 16,1% |
| Five Drugs | 1 | 16,1% |
| Total | 62 | 100% |
| Table 6: Distribution by Drug Involved. | ||
| Type of Drug | Frequency | Percentage |
| Amoxicillin | 1 | 1,6% |
| Chloroquine | 6 | 9,7% |
| No known allergy | 55 | 88,7% |
The molecules to which patients were allergic were essentially chloroquine (6 times) and amoxicillin (1 time). The main molecules involved were: antibacterial sulfamides (24 cases), allopurinol (8 cases), antimalarials (22 cases). This was self-medication in 29 cases or 46.77%(Table 7).
| Table 7: Distribution by Drug Intake. | ||
| Médicaments suspects | Frequency | Percentage |
| Co-trimoxazole | 16 | 25,85% |
| Sulfadoxine/ pyrimethamine | 12 | 19,35% |
| Allopurinol | 5 | 8,06% |
| None | 3 | 4,83% |
| Lactam Coumpounds | 3 | 4,83% |
| Neuroleptics | 3 | 4,83% |
| Antiretrovirals | 2 | 3,22% |
| Trioleandomycin | 2 | 3,22% |
| Dapsone | 1 | 1,6% |
| Plaquenil | 11 | 1,6% |
| Authers | 14 | 22,58% |
| Total | 62 | 100% |
This was self-medication in 29 cases or 46.77% (Table 8).
| Table 8: Distribution by Type of Drug Intake. | ||
| Type of Drug Intake | Frequency | Percentage |
| medical Prescription | 33 | 53,22% |
| Self-medication | 29 | 46,77% |
| Total | 62 | 100% |
The clinical aspects observed were fixed erythema pigment or EPF (26 cases), Steven Johnson (16 patients including 7 with ocular involvement), - skin rash (15 cases), toxic epidermal necrolysis (4 cases) and finally a Drug reaction with eosinophilia and systemic syndrome (DRESS) 1 case (Table 9).
| Table 9: Distribution by clinical diagnosis. | ||
| Diagnosis | Frequency | Percentage |
| Fixed drug eruption | 26 | 41,9% |
| Rash | 15 | 24,2% |
| Steven Johnson Syndrome | 16 | 25,8% |
| Lyell Syndrome | 4 | 6,5% |
| DRESS syndrome | 1 | 1,6% |
| Total | 62 | 100% |
More than half of the patients visited the first few days after the first symptoms (Tables 10,11).
| Table 10: Distribution by Time Taken Prior to Consultation. | ||
| Time | Frequence | Percentage |
| 0-1 day | 35 | 56,4% |
| 2-6 days | 15 | 24,19% |
| 7-15 days | 12 | 19,35% |
| Total | 62 | 100% |
| Table 11: Distribution by evolution. | ||
| Evolution | Frequence | Percentage |
| Healing with sequelae | 2 | 3,2% |
| Death | 1 | 1,6% |
| Healing without sequelae | 56 | 90,3% |
| Lost sight of | 3 | 3,2% |
| Total | 62 | 100% |
The progression of the disease was marked by healing without sequelae in 56 patients (90.3%), death in one patient (75-year-old patient). Finally, three patients were lost sight of.
The average age of our patients was 30 years. This young age found in our series is comparable to that of Safiatou, et al. who reported an average age of 31.4 [6]. On the other hand, in the European and Asian series, toxidermis predominates in older subjects because of the frequent poly medication in these subjects [2,7]. In our series, as in the one reported by Özkaya-Bayazit and Harugeri [7, 8], the frequency of toxidermis was the same in both sexes. On the other hand, in the European series, there was a predominance of women probably explained by their susceptibility to develop a toxidermy [2]. The Peuhl ethnic group was the most represented, with a frequency of 22.6%.There is no explanation for this predominance which could be a reflection of the consulting population or a mere coincidence. The majority of the patients came from Bamako. This is related to the proximity of the service, which represents, at the national and even sub-regional level, the largest centre for skin disease management. Clinically, Atopy: A notion of atopy was found in 3.2% of subjects. This result differs from that of Weeranut which reported an atopy rate of 20.9% [9]. This low proportion of atopic in our study may be explained by the difficulty of collecting information. Among the reasons for taking drugs, malaria was the main reason for taking drugs in our patients. This is easily explained by the high prevalence of this condition and the easy attribution of all the conditions to this source. Self-medication is a common practice in developing countries, particularly in Mali. In our series it was 46.77% against 51% in the study of Safiatou [6]. The proliferation of street drug outlets (on-street pharmacies) and the easy availability of non-prescription drugs make self-medication a common practice. Maculopapular exanthema is the most commonly reported clinical form of toxiderma in the literature [2]. However, in our series, fixed erythema pigment was the most common clinical form. Similar results were observed by other authors [6,7]. The onset of lesions ranged from 1 to 3 weeks. These data are compatible with the results of previous work, notably those of Roujeau, et al. and Krebs, et al. [2,10]. They generally correspond to the time required for the body to become aware of the drug. The majority of our patients consulted from the first day of the rash. This is related to the disturbing and brutal nature of the affection. Among the severe clinical forms of toxiderma in our series, Steven Johnson syndrome was the most common form. This predominance of the SJS is found in India [8] and Madagascar [11].
With 34.37% and 61.53% respectively. On the other hand, our results contradict those reported by Safiatou who found 2.35% of SJS (2/85) and Weeranut who found 8.4% (16/191) [6.10]. These differences are explained by the specificities of these different studies. The anti-infectious sulfamides were the most incriminated molecules in the occurrence of toxidermies in our patients: cotrimoxazole was found 16 times (25.85%), sulfadoxine pyrimethamine 12 times (19.35), Allopurinol 5 times (8%) and betalactamines 3 times. Our results are in line with the work carried out by Özkaya and Collaborateurs who found cotrimoxazole in 63.8% of patients with fixed erythema pigment [7]. In the study of Safiatou [6]. Paracetamol was responsible for toxicity in 23.08% of patients; penicillin was found in several authors [12-14]. This predominance of anti-infectious sulfamides is explained on the one hand by the high consumption of these molecules linked to its use in palustrine syndromes, respiratory and digestive diseases, and on the other hand, because of its availability both in the stores and in the parallel market of our cities. In our series, 45.2% (28/62) of patients had consumed at least 2 medications before the onset of the rash. In the series published by Aguèmon on Lyell syndrome in intensive care settings, the majority of patients used several medications (27.42%) [13]. The seroprevalence of HIV in our study was 6.5% (4/62). In the Weeranut study, it was 22% (22/1541) [9]. The relationship between immunosuppression and HIV has been the subject of much work [4]. The risk of developing toxiderma is increased in HIV-infected patients. Recovery without sequelae was noted in 90.3% (56/62) of cases. For the rest, 2 patients had ocular sequelae (1 woman aged 60 and 1 man aged 17), 3 patients were lost of sight and 1 patient died during hospitalization (woman aged 70). The incidence of eye damage was estimated at 30.81% in France and 56% in Morocco.
At the end of our study, it is clear that toxidermis remains common in developing countries such as sub-Saharan Africa. This high frequency is probably related to malaria endemicity in this region requiring the use of the antimalarial responsible for the toxidermis and the high frequency of self-medication.
The authors gratefully thank all patients for their acceptance to participate in this study. We would also like to think Professor Ousmane Faye for this unconditional support for malian young researchers. Warmful thanks to the administration, for all the facilities obtained to carry out the present study.
- Privat Y. Toxidermies médicamenteuses, diagnostic et prévention. Ann Dermatol Venereol. 2003; 130: 159-153.
- Roujeau JC, Wolkenstein P. Réactions cutanées aux médicaments. In Dermatologie et infections sexuellement transmissibles ; 4èmeé dition Masson. Paris. 2000; 385-392.
- Ramorasata JA, Raveloson NE, Tohaina D, et al. Caractéristiques épidémio-cliniques des nécrolyses épidermiques toxiques dans le service de réanimation de l’Hôpital de Soavinandriana Antananarivo. Rev Anest Réa Urg. 2009; 1: 21-25.
- Atadokpede F, Yedomon H, Adegbidi H, Sehonou JJ, Azondekon A, et al. Mucocutaneous manifestations of human immunodeficiency virus infection in Cotonou, Benin. Med trop. 2008; 68: 273-276. PubMed: https://pubmed.ncbi.nlm.nih.gov/18689320/
- Begaud B, Evreux JC, Jouglard J, G Lagier. Imputation of the unexpected or toxic effects of drugs. Actualization of the method used in France. Therapie. 1985; 40: 111-118. PubMed: https://pubmed.ncbi.nlm.nih.gov/4002188/
- Safiatou I. Réactions cutanéo-muquqeuses d’origine médicamenteuse, thèse de médicine Fmpos n°07M197.
- Özkaya E. Specific site involvement in fixed drug eruption. J Am Acad. Dermatol. 2003; 49: 1003-1007. PubMed: https://pubmed.ncbi.nlm.nih.gov/14639376/
- Harugeri BM, Sanmukhani J, Patel T, Paliwal N, Shah H, Tripathi C, et al. Drug induced Stevens - Johnson syndrome, toxic epidermal necrolysis, and SJS-TEN overlap: A multicentric retrospective study. J Postgrad Med. 2011; 57: 115-119. PubMed: https://pubmed.ncbi.nlm.nih.gov/21654132/
- Weeranut C, Leena C, Kanokvalai K, Jongjarearnprasert K, Dhana N. Cutaneous adverse reactions to sulfonamide antibiotics. Asian Pac J Allergy Immunol. 2011; 29: 284-289. PubMed: https://pubmed.ncbi.nlm.nih.gov/22053600/
- Krebs A, Boillat-Armagni C, Saurat JH. Réactions cutanées aux médicaments. In: Dermatoses des états d'hypersensibilité 2ème ed. Paris: Masson. 1990: 911.
- Ramorasata JA, Raveloson NE, Tohaina D. Caractéristiques épidémio-cliniques des nécrolyses épidermiques toxiques dans le service de réanimation de l’Hôpital de Soavinandriana Antananarivo. Rev Anest Réa Urg. 2009; 1: 21-25.
- Khaled A, Kharfi M, Ben Hamida M, El Fekih N, El Aidli S, et al. Cutaneous adverse drug reactions in children. A series of 90 cases. Tunis Med. 2012; 90: 45-50. PubMed: https://pubmed.ncbi.nlm.nih.gov/22311448/
- Aguèmon AR, Houngbé F, Yaméogo TM. Nécrolyse épidermique toxique, revue des cas Observés dans le service de réanimation du centre national hospitalier et universitaire de Cotonou. Ann Fr Anesth Réanim. 2006; 25: 505-509.
- Bahadoran P, Castanet J, Lacour LP, Perrin C, Del Giudice P, et al. Pseudo-dermatomyositis induced by long-term hydroxyurea therapy: report of two cases. Br J Dermatol. 1996; 134: 1161-1163. PubMed: https://pubmed.ncbi.nlm.nih.gov/8763456/