Research Article
Clinical significance of Vibration Anesthesia on reducing pain of Ring-Block (Subcutaneous Injections) in the patients undergoing Hair Restoration Surgery

Muhammad Ahmad* and Mohammad Humayun Mohmand*
Cosmetic Plastic Surgeon, Hair Transplant Institute, Islamabad, Pakistan
*Address for Correspondence: Muhammad Ahmad, Plastic and Hair Restoration Surgeon, Aesthetic Plastic Surgery and Hair Transplant Institute, H. 1B, Main Kohistan Road, Sector F-8/3, Islamabad, Pakistan, Tel: +92-300-5239465; Email: [email protected]
Dates: Submitted: 29 September 2017; Approved: 17 October 2017; Published: 18 October 2017
How to cite this article: Ahmad M, Mohmand MH. Clinical significance of Vibration Anesthesia on reducing pain of Ring-Block (Subcutaneous Injections) in the patients undergoing Hair Restoration Surgery. Ann Dermatol Res. 2017; 1: 001-005. DOI: 10.29328/journal.adr.1001001
Copyright License: © 2017 Ahmad M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Pain is a complex phenomenon which is unpleasant. Different cosmetic procedures are associated with varying degrees of pain. Various modalities are adopted to decrease the severity of pain. The commonly used is the administration of analgesics (opioid or non-steroidal). The pain is carried to the brain by pain fibres. There are various theories about the pain [1,2]. Many attempts have been undertaken to find the modalities which decrease the perception of pain by the brain. The famous ‘gate theory’ was proposed in 1965 by Melzack et al. [3]. It was proposed that the pain experience can be reduced by the activation of nerve fibres that conduct non-toxic stimuli. The theory suggested that the stimulation of larger diameter fibres (A-beta) can close a neural ‘gate’ to nocioceptive signals and can reduce the perception of the pain. The ‘gate’ is proposed to lie within the spinal cord/brainstem and inhibits the transmission of nocioceptive action potentials to higher centres in the central nervous system [4]. The “post-synaptic inhibitory and fascilitatory mechanism” provide a basis for explaining the pain reducing strategies such as rubbing the painful area or applying cold or vibration to decrease the perception of the pain. Various topical irritants used in a few ‘magic’ creams also work on the same principle.
Every effort is made to decrease the perception of pain in cosmetic surgery procedures especially hair restoration. A surgeon who can perform a hair restoration without pain has an edge over his competitors. The potential patients undergoing hair restoration are very anxious about the pain level to be perceived during the procedure. Vibration anaesthesia is becoming increasing used in hair restoration to decrease pain perception. Various recent studies have demonstrated the effective use if vibrations to decrease the pain of local anaesthesia injections [5,7]. The pain of the injection has basically two components; the first is the actual needle prick and second is the discomfort felt due to the tissue stretch by the local anaesthetic drugs [8].
The following study was conducted to compare the pain level of ring block in the patients undergoing hair restoration with and without the use of vibration.
Materials and Methods
The study was undertaken in a private hair restoration center in adult patients undergoing 1st session of hair transplant surgery. Written informed consent was obtained from all the patients were given detailed per-operative consultation about the procedure, injection and outcome. First generation cephalosporins and diazepam 10 mg were given orally about 15 minutes before the procedure. The patients underwent strip harvest technique or follicular unit extraction. The scalp on the forehead was divided into 2 halves from midline. Each side was assigned to one of the injection techniques A or B randomly. The decision about the first technique was also undertaken randomly. The solution injected on each side contained 20ml of 2% Xylocaine, 0.5 ml of adrenaline and 40ml of normal saline. A separate syringe with 30oG needle was used on each side.
Injection technique A (without vibration)
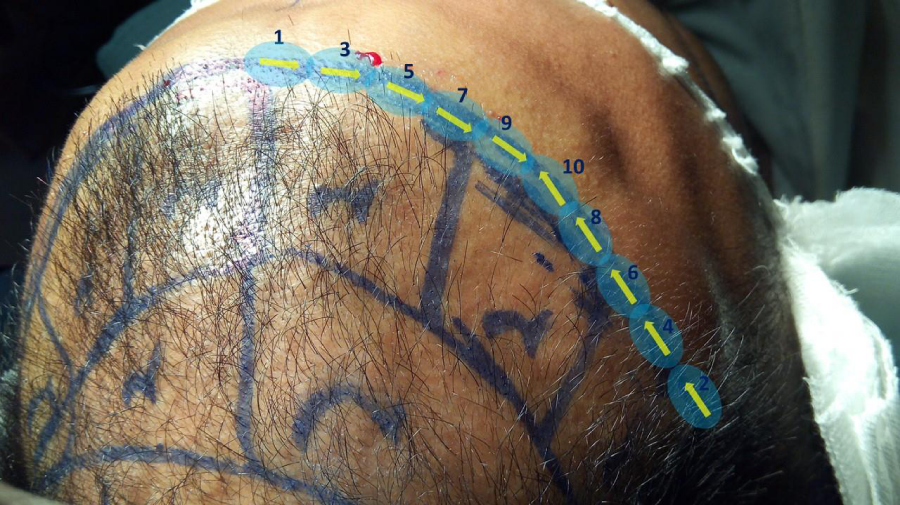
The 1st injection was given in the midline and directed towards the ear. The 2nd injection was given at the juncture of upper border of temporal with the frontal hairline. All the later injections were administered alternatively. First a weal of local anaesthetic was raised injection about 0.5 ml of the solution. The nest injection was given at the end of the weal (Figure 1). In each prick, 0.5 ml of the solution was injected.
Injection technique B (with vibration)
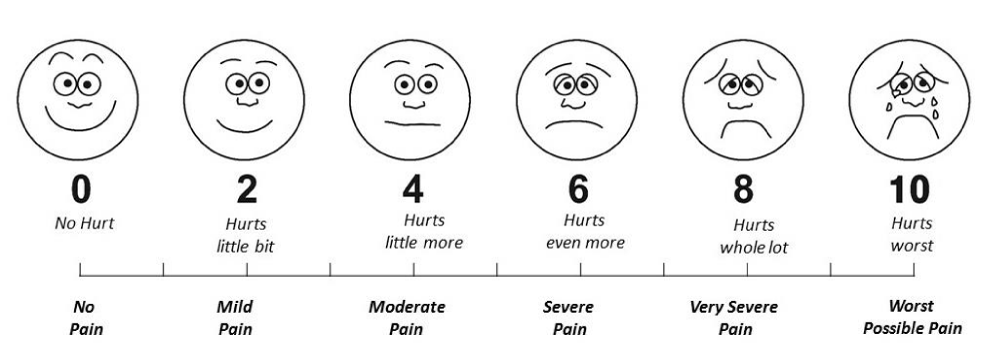
First of all, the vibrator was started and placed over the site for about 3-5 seconds before the injection. The needle was inserted slowly and about 0.5 ml of the solution was injected in the midline. The 2nd injection was given at the juncture of upper border of temporal with the frontal hairline using the vibrator (Figure 2). The rest of the injections were carried out alternatively through the weal produced of the previous injection. The injections were administered by the first author therefore the speed of injection was kept constant in all the patients. At the end of the injections on each side, the patient was asked about the level of pain according to the Wong Baker Faces Pain Scale (Figure 3) [9]. All the data was then analyzed statistically using ‘Stats tester’ © version 2.0.1, 2016-17, BMP Group, Saitama, Japan.
Results
Twenty-five patients were included in the study. The mean age of the patients was 34.52 years (range, 24-52 years). The average pain score without vibration was 4.56 (range, 1-8) whereas the average pain score with vibrator was 2.96 (range, 1-5). Majority of the patients (44%) undergoing injections without vibrator had score ‘5’ or ‘6’ whereas majority (60%) had score ‘3’ or ‘4’ with the vibrator (Table 1). About 44% of the patients were smokers. The average pain score in non-smokers was 4.14 without vibrator and 2.57 with vibrator. The average pain score in smokers was 5.09 without vibrator and 3.45 with vibrator (p< 0.05).
| Table 1: Patients’ data. | ||||
| S. No. | Age | Score without Vibrator | Score with Vibrator | Co-morbid condition |
| 1 | 25 | 5 | 3 | Non- Smoker |
| 2 | 27 | 6 | 4 | Non- Smoker |
| 3 | 31 | 4 | 1 | Non- Smoker |
| 4 | 33 | 2 | 1 | Non- Smoker |
| 5 | 39 | 4 | 3 | Non- Smoker |
| 6 | 39 | 6 | 3 | Non- Smoker |
| 7 | 36 | 3 | 2 | Non- Smoker |
| 8 | 52 | 2 | 2 | Non- Smoker |
| 9 | 36 | 4 | 2 | Non- Smoker |
| 10 | 34 | 3 | 1 | Smoker |
| 11 | 29 | 4 | 3 | Non- Smoker |
| 12 | 26 | 6 | 4 | Smoker |
| 13 | 30 | 5 | 3 | Smoker |
| 14 | 32 | 5 | 4 | Smoker |
| 15 | 32 | 6 | 3 | Smoker |
| 16 | 35 | 6 | 4 | Smoker |
| 17 | 37 | 5 | 4 | Smoker |
| 18 | 41 | 6 | 4 | Non- Smoker |
| 19 | 44 | 1 | 2 | Smoker |
| 20 | 33 | 8 | 5 | Non- Smoker |
| 21 | 31 | 4 | 3 | Non- Smoker |
| 22 | 35 | 3 | 3 | Smoker |
| 23 | 40 | 3 | 3 | Smoker |
| 24 | 28 | 7 | 5 | Smoker |
| 25 | 38 | 6 | 2 | Smoker |
Discussion
Pain is an important factor in hair restoration surgery. The potential patients are anxious about the degree of pain to be expected during the surgery. There are multiple factors which are associated with the degree of pain. The needle gauge (length and diameter), bolus of the drug injected, the anatomic areas, the composition of the local anaesthetic, temperature, pH etc, all are significant factors. The pain sensation is transmitted by two main types of fibres (myelinated A-delta fibres and type C fibres). The touch sensation is carried by A-beta fibres. The ‘gate’ theory of pain postulated that there is an interaction between pain fibres and touch fibres input at the spinal cord level and a non-painful stimulus can block the transmission of a painful stimulus [3]. The vibration also stimulates the mechanoreceptors and primary nerve endings of the muscle spindle too [10,11]. The stimulus which reaches the brain first is perceived first [3]. Various studies have been mentioned in which vibration anaesthesia has been used to reduce the pain, however there are a few studies which also describe its use in hair restoration surgery [12,13].
The vibrations applied before the noxious stimulus (like injection) reduces the intensity of the pain perceived by the brain. We also used vibration about 3-5 seconds before the injection was given. The local anaesthetic injection has 2 components. The 1st component of actual ‘needle prick’ is blocked but the vibrations applied [8]. The 2nd component of pain is due to the injection of anaesthetic drug and is dependent on various factors like composition, the volume, temperature, pH and speed of injection. This component of pain can also be reduced by the vibrations as it massages the local area and helps in the fluid dissolution into the surrounding tissues. The audible sounds produced by the vibrator also helps to divert the attention of the patient. The size of the needle and the injection speed influence the severity of pain perceived by the patients.
The use of vibration just before the injection reduces the pain as shown in many other studies [14,15]. In the current studies the average pain score was 4.56 without the use of vibrator and 2.96 with the vibrator (p< 0.05). We also postulate that the vibration applied just prior to the injection needle, actually divert the attention of the patient as well as helps to reduce the degree of pain felt. In another study by the author, the average pain score of supraorbital/supratrochlear (SO/ST) nerve block was 4.6 without the vibrator and 2.4 with the vibrator which are comparable to the results of the current study. Moreover, the comparison of both the studies also revealed that there was almost no clinically significant difference of pain between two techniques. It also ruled out the belief by many surgeons that the SO/ST nerve blocks are very much painful than the ring block or subcutaneous injections (4.56 in subcutaneous ring block injections vs 4.6 in SO/ST nerve block without vibration anaesthesia and 2.96 in subcutaneous ring block injections vs 2.4 in SO/ST nerve blocks with vibrations applied). The same observation was also seen in another study by the author [16].The current study indicates that the vibration can reduce the pain of the injection dramatically.
References
- Dubner R, Sesele BJ, Storey AT. The neural basis of oral and facial function. New York: Plenum. 1978. 1979; 75: 695. Ref: https://goo.gl/JK63qN
- Moayedi M, Davis KD. Theories of pain from specificity to gate control. J Neurophysiol. 2013; 109: 5-12. Ref: https://goo.gl/ZrRAQP
- Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965; 150: 971-979. Ref: https://goo.gl/vbeHwh
- Nanitsos E, Vartuli R, Forte A, Dennison PJ, Peck CC. The effect of vibration on pain during local anaesthesia injections. Aust Dent J. 2009; 54: 94-100. Ref: https://goo.gl/Gr5gF9
- Shahidi Bonjar AH. Syringe micro vibrator (SMV) a new device deing introduced in dentistry to alleviate pain and anxiety of intraoral injections and a comparative study with a similar device. Ann Surg Innov Res. 2011; 5: 1. Ref: https://goo.gl/sNxbgB
- Nasehi A, Bhardwaj S, Kamath AT, Gadicherla S, Pentapati KC. Clinical pain evaluation with introral vibration device during local anaesthetic injections. J Clin Exp Dent. 2015; 7: 23-27. Ref: https://goo.gl/7E8qSt
- Sharma P, Czyz CN, Wulc AE. Investigating the efficacy of vibration anaesthesia to reduce pain from cosmetic Botulinum toxin injections. Aesthet Surg J. 2011; 31: 966-971. Ref: https://goo.gl/tbjToJ
- Ahmad M, Mohmand MH. Use of vibration anaesthesia in hair restoration surgery. J Pak Assoc Dermatol. 2017; 27.
- Ref.: https://goo.gl/lg5y3n .
- Johansson RS, Landstrom U, Lundstrom R. Responses of mechanoreceptive afferent units in the glabrous skin of the human hand to sinusoidal skin displacements. Brain Res. 1982; 244: 17-25. Ref: https://goo.gl/yCFH2A
- Hasan Z, Houk AC. Analysis of response properties of deeferented mammalian spindle receptors based on frequency response. J Nerophysiol. 1975; 38: 663-672. Ref: https://goo.gl/w537Un
- Kohn T, Zari S. Local anaesthesia techniques in hair restoration surgery. J Cut Med Surg. 2016; 20: 610-612. Ref: https://goo.gl/8mp4pt
- Seager DJ, Simmons C. Local anaesthesia in hair transplantation. Dermatol Surg. 2002; 28: 320-328. Ref: https://goo.gl/q7Ncwo
- Cem Ungor1, Emre Tosun, Ezher Hamza Dayisoylu, Fatih Taskesen, Figen Cizmeci Senel. The effects of vibration on pain and anxiety during local anaesthesia administration. JSM Dent. 2014; 2: 1022. Ref: https://goo.gl/UwPGr5
- Fayers T, Morris DS, Dolman PJ. Vibration-assisted anaesthesia in eyelid surgery. Ophthalmology. 2010; 117: 1453-1457. Ref: https://goo.gl/wTK4LF
- Muhammad Ahmad, Humayun Mohmand. Nerve blocks or subcutaneous injections: comparison of pain levels in patients undergoing hair transplant surgery. Pak J Plast Surg 2015; 4:19-22. Ref: https://goo.gl/y7fT3E